The liver is one of the body’s most hardworking organs, performing over 500 vital functions, from detoxifying blood to producing essential proteins and aiding digestion. Given its critical role in maintaining overall wellness, monitoring its health is paramount. This is where the liver function test (LFT), also known as a liver panel, comes in.
Understanding your liver’s status is a proactive step in managing your well-being and detecting issues early. The liver function test is a simple, yet incredibly powerful blood test that measures specific enzymes and proteins in your blood. These measurements provide a snapshot of how well your liver is operating and whether it has suffered damage.
If you’ve ever wondered what those acronyms like AST, ALT, and ALP mean, or what an abnormal liver function test result signifies, this comprehensive guide is for you. We’ll demystify the entire process, empowering you to take control of your liver health.
Table of Contents
What Are Liver Function Tests?
A liver function test (LFT) is a set of blood tests that healthcare providers use to assess the health and performance of the liver. Although the name suggests these tests measure function exclusively, they primarily check for liver cell damage or inflammation.
When liver cells (hepatocytes) are injured, they release certain enzymes into the bloodstream. Measuring the levels of these enzymes gives doctors a reliable indicator of liver damage. Furthermore, the LFT panel also measures substances that the liver is responsible for producing or processing.
These blood tests are routinely ordered as part of a general check-up, especially if a patient is presenting with symptoms that suggest potential liver disease, such as jaundice, fatigue, or abdominal pain.
The Core Purpose of LFTs
The fundamental goal of ordering a liver function test is three-fold:
- Screening: To check for evidence of liver damage or liver disease in people with no symptoms but who may be at risk (e.g., heavy drinkers, those with a family history of liver problems).
- Diagnosis: To help identify the specific cause of liver damage, such as hepatitis, fatty liver disease, or bile duct obstruction.
- Monitoring: To track the progress of an existing liver disease or to assess the effectiveness and potential side effects of medications.
Also Read: Discover 5 Amazing Blood Check Services Near You: A Comprehensive Guide to Local Health Solutions
Importance of Liver Function Tests in Health Monitoring
Monitoring your liver health is critical because the liver is incredibly resilient and often doesn’t show symptoms until significant damage has occurred. The liver has a remarkable capacity to regenerate, which means minor injuries often heal unnoticed. However, persistent or severe damage can lead to chronic conditions like cirrhosis or liver failure.
Regular LFTs serve as an early warning system, allowing for interventions before serious, irreversible damage takes place. Early detection of elevated liver enzymes can lead to lifestyle changes or medical treatment that can completely reverse conditions like early-stage fatty liver.
Detecting Silent Liver Disease
Many people live with conditions like Non-Alcoholic Fatty Liver Disease (NAFLD) or chronic viral hepatitis for years without knowing it. These are “silent killers” because they often produce no noticeable symptoms in the early stages.
- Early Intervention: An abnormal liver function test result can prompt further testing (like an ultrasound or biopsy) to catch these silent diseases in time.
- Medication Safety: LFTs are essential for monitoring patients on medications known to be potentially toxic to the liver, ensuring the drug’s benefit outweighs any harm.
- Overall Health Snapshot: Elevated liver enzymes are sometimes the first clue that a person has a related metabolic syndrome, such as diabetes or high cholesterol, prompting a broader health assessment.
Common Liver Function Tests Explained
A standard liver function test panel typically includes several specific measurements. These are broadly categorized into tests that measure liver injury (enzymes) and tests that measure the liver’s synthetic ability (proteins and bilirubin).
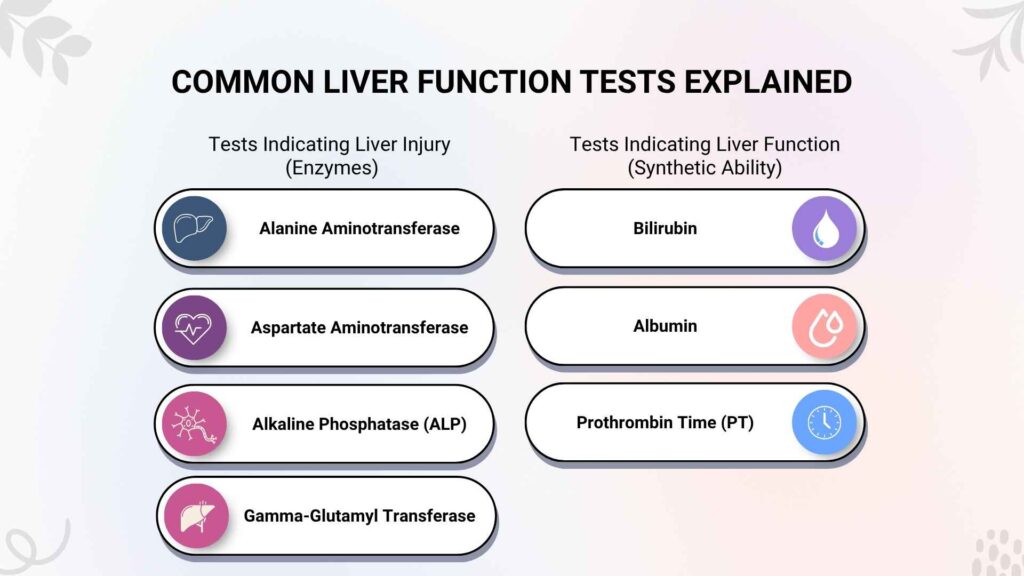
Tests Indicating Liver Injury (Enzymes)
These enzymes are usually contained within liver cells. High levels in the blood suggest that liver cells have been damaged and “leaked” their contents.
Alanine Aminotransferase (ALT)
- What it is: An enzyme found predominantly in the liver. It’s considered the most specific indicator of liver inflammation or damage.
- What high levels mean: Primarily indicative of acute hepatitis (viral or drug-induced) or fatty liver disease. High ALT usually points to injury of the liver cells themselves.
Aspartate Aminotransferase (AST)
- What it is: An enzyme found in the liver, but also in smaller amounts in the heart, muscle, and kidneys.
- What high levels mean: Often rise alongside ALT, but high AST with only mildly elevated ALT may suggest damage originating from muscles or the heart. If AST is significantly higher than ALT, especially with heavy alcohol use, it can be a classic indicator of alcoholic hepatitis.
Alkaline Phosphatase (ALP)
- What it is: An enzyme found in the bile ducts, liver, and bone.
- What high levels mean: Suggests a problem with the bile ducts (cholestasis)—such as a blockage from a gallstone or tumor—or bone disease. If accompanied by high GGT, the cause is very likely liver or bile duct related.
Gamma-Glutamyl Transferase (GGT)
- What it is: Another enzyme concentrated in the liver cells and bile ducts.
- What high levels mean: Often measured with ALP. A high GGT combined with high ALP strongly confirms that the high ALP is due to liver/bile duct problems, rather than bone disease. It is also often elevated by alcohol consumption, certain drugs, and fatty liver disease.
Tests Indicating Liver Function (Synthetic Ability)
These tests measure substances the liver produces or processes, thus directly reflecting its synthetic and excretory capacity.
Bilirubin
- What it is: A yellow pigment that is a waste product from the normal breakdown of red blood cells. The liver processes (conjugates) and excretes it via bile.
- What high levels mean: Can cause jaundice (yellowing of the skin/eyes). High levels can indicate several issues: the liver isn’t processing bilirubin correctly, there’s too much breakdown of red blood cells (hemolysis), or there is a blockage in the bile ducts preventing excretion.
Albumin
- What it is: The main protein produced by the liver. It helps transport hormones and drugs and maintains fluid balance in the body.
- What low levels mean: Since albumin has a relatively long half-life, low levels typically indicate a chronic, long-term problem with the liver’s ability to synthesize proteins. It can be a sign of advanced chronic liver disease.
Prothrombin Time (PT) / International Normalized Ratio (INR)
- What it is: Measures how quickly your blood clots. Clotting factors are proteins synthesized by the liver.
- What a high result (longer time) means: Indicates that the liver is not producing enough clotting factors. A prolonged PT/INR is a sensitive measure of the liver’s synthetic failure and is often a sign of significant, severe liver dysfunction.
Also Read: CT Angiography Insurance Coverage: Avoid Surprise Costs
Interpreting Liver Function Test Results
Interpreting a liver function test is not about looking at a single number; it’s about seeing the complete picture. The patterns of elevation across the different tests provide the most valuable diagnostic clues.
Understanding the Normal Range
The “normal range” is a reference interval (usually provided in your lab report) derived from testing a large population of healthy people. Results falling outside this range are considered abnormal. However, the normal range can vary slightly based on the specific laboratory and the testing equipment they use.
Key takeaway: A result slightly outside the range isn’t necessarily a crisis, but it warrants a discussion with your healthcare provider.
Key Patterns of Abnormal Liver Results
The pattern of the elevated liver enzymes helps the doctor differentiate between the causes of damage:
| Pattern of Elevation | Primary Indication | Examples of Conditions |
| Hepatocellular (ALT & AST dominant) | Damage to the liver cells (hepatocytes). | Viral Hepatitis (A, B, C), Fatty Liver Disease, Autoimmune Hepatitis, Drug/Toxin Injury. |
| Cholestatic (ALP & GGT dominant) | Blockage or injury to the bile ducts. | Gallstones, Tumors (pancreatic/bile duct), Primary Biliary Cholangitis (PBC). |
| Impaired Synthesis (Low Albumin/High INR) | Severe, chronic loss of liver function. | Cirrhosis (Scarring), Acute Liver Failure. |
Factors Affecting Liver Function Test Outcomes
It’s crucial to understand that an abnormal liver function test doesn’t always mean you have chronic liver disease. Many factors can temporarily or harmlessly skew the results.
Non-Liver Related Influences
- Muscle Injury: Intense exercise, particularly resistance training, can significantly raise AST and, to a lesser extent, ALT. These enzymes are also found in muscles.
- Medications: Many prescription and over-the-counter drugs, including statins, antibiotics, and even high doses of acetaminophen (Tylenol), can cause temporary or sustained elevations in liver enzymes.
- Alcohol: Recent heavy alcohol consumption can cause significant, often transient, elevations, especially in AST and GGT.
- Diet/Supplements: Certain dietary supplements, particularly herbal remedies (e.g., Kava, high doses of green tea extract), and rapid weight loss can sometimes affect LFT results.
Also Read: MRI vs. CT Scan: What’s the Difference and Which Do You Need?
When Should You Get a Liver Function Test?
LFTs are a standard part of routine healthcare, but there are specific symptoms and risk factors that necessitate them.
Symptoms That Prompt an LFT
Your doctor will likely order a liver function test if you exhibit any of the following symptoms:
- Jaundice: Yellowing of the skin and eyes (due to high bilirubin).
- Abdominal Pain or Swelling: Especially on the upper right side (where the liver is located).
- Nausea, Vomiting, and Loss of Appetite: Non-specific symptoms that can indicate liver distress.
- Unexplained Fatigue or Weakness: Chronic liver problems often present with profound fatigue.
- Dark Urine or Pale Stool: Signifying problems with bilirubin excretion.
Risk Factors Requiring Screening
Even without symptoms, an LFT is recommended if you have certain risk factors:
- History of heavy or chronic alcohol use.
- Exposure to or diagnosis of Hepatitis B or C.
- Obesity, Type 2 Diabetes, or High Cholesterol (key risk factors for Fatty Liver Disease).
- A family history of liver disease.
- Monitoring patients on hepatotoxic (liver-damaging) medications.
Preparing for a Liver Function Test
The liver function test is simple, but preparation can ensure the most accurate results.
Simple Preparation Steps
- Fasting (Usually Required): Most LFT panels require fasting for 10–12 hours before the blood draw. This is mainly to ensure accurate triglyceride and glucose readings (often drawn alongside the LFT), as high-fat meals can affect ALP and bilirubin levels.
- Medication Review: Inform your doctor about all prescription drugs, over-the-counter medications, and supplements you are taking. They may advise temporarily stopping certain non-essential supplements.
- Avoid Alcohol: Refrain from consuming alcohol for at least 24–48 hours before the test, as alcohol can temporarily spike liver enzymes, particularly GGT.
- Limit Intense Exercise: Avoid strenuous physical activity 24 hours prior, as it can elevate AST and ALT.
Also Read: Different Types of Ultrasound Scans and When You Need Them
Understanding Abnormal Results and Next Steps
An abnormal LFT is a flag, not a final diagnosis. It simply indicates that something is stressing the liver.
The Follow-Up Process
If your liver function test shows significant or persistent abnormalities, your physician will initiate a systematic follow-up plan:
- Re-testing: The doctor may first repeat the LFT in a few weeks to see if the levels normalize on their own, especially if no clear cause is found.
- Additional Blood Tests: Tests for specific viruses (Hepatitis B/C), autoantibodies (for autoimmune hepatitis), or iron/copper levels (for hemochromatosis/Wilson’s disease).
- Imaging: An abdominal ultrasound is a common next step to check the liver’s size, look for fatty liver (steatosis), and check for bile duct obstructions.
- Lifestyle Changes: Depending on the cause, the most important step is often counseling on reducing alcohol, improving diet, and increasing physical activity to manage conditions like fatty liver.
Conclusion: Taking Control of Your Liver Health
The liver function test is an invaluable tool for preventative health and early diagnosis. By understanding what these tests measure—from enzymes like ALT and AST to proteins like albumin—you gain the knowledge to advocate for your own well-being. Don’t fear the test; use it as a powerful guide. Talk to your doctor today about your risk factors and ensure regular screening is part of your health regimen.
Ready to prioritize your liver? Schedule a consultation with your primary care physician to discuss your liver health and determine if a liver function test is right for you. Proactive care starts with knowledge.
Also Read: Things to Know Before Booking a Blood Test at Home
Frequently Asked Questions
Q1: What is the single most common cause of elevated liver enzymes (ALT/AST)?
The single most common cause of mildly to moderately elevated liver enzymes (specifically ALT and AST) in the Western world is Non-Alcoholic Fatty Liver Disease (NAFLD), now often referred to as Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD).
NAFLD is directly linked to features of metabolic syndrome, including obesity, Type 2 diabetes, high cholesterol, and insulin resistance. In this condition, excess fat accumulates in liver cells, causing inflammation and subsequent injury, which leads to the leakage of enzymes into the bloodstream. Because NAFLD is often asymptomatic in its early stages, elevated liver enzymes on a routine blood test are frequently the first sign of the disease. Early detection is crucial because, left unmanaged, NAFLD can progress to more serious conditions like fibrosis and cirrhosis.
Q2: What is the difference between AST and ALT, and why does it matter?
Both ALT (Alanine Aminotransferase) and AST (Aspartate Aminotransferase) are key liver enzymes that indicate hepatocellular (liver cell) damage when found at elevated levels in the blood. The key difference lies in their tissue distribution:
- ALT: This enzyme is found primarily and in high concentration within the liver. Therefore, elevated ALT is considered the more specific marker of liver cell injury or inflammation.
- AST: While also present in the liver, AST is found in significant amounts in other tissues, including the heart, skeletal muscles, and kidneys.
The ratio between the two is often clinically significant:
- ALT > AST: This is the most common pattern and suggests non-alcoholic fatty liver disease, viral hepatitis (Hepatitis B or C), or drug-induced liver injury.
- AST > ALT (typically a ratio of 2:1 or more): This pattern is a classic indicator of alcoholic hepatitis or cirrhosis, though it can also be seen with severe muscle damage.
Q3: Do I need to fast before a liver function test (LFT)?
Yes, most labs recommend fasting for 10–12 hours before a liver function test (LFT) or a comprehensive metabolic panel.
While the core liver enzymes (ALT and AST) are usually unaffected by a recent meal, fasting is often necessary for two primary reasons:
- Concurrent Tests: LFTs are commonly ordered alongside glucose and cholesterol tests, both of which do require fasting for accurate measurement.
- Bilirubin and ALP: Eating, especially a high-fat meal, can temporarily affect levels of bilirubin and Alkaline Phosphatase (ALP). Fasting ensures the most consistent and accurate baseline measurements for the complete panel, preventing false highs that might lead to unnecessary follow-up tests. It’s always best to confirm the fasting requirement with your healthcare provider or the lab drawing the blood.
Q4: Can stress or intense exercise raise my liver function test results?
Yes, both factors can influence LFT results, although intense exercise is the more common and reliable culprit.
- Intense Exercise: Strenuous physical activity, particularly weightlifting or prolonged endurance exercise performed within 24 hours of the blood draw, can temporarily cause a significant rise in AST and sometimes ALT. This is because these enzymes are released from damaged skeletal muscle tissue following an intense workout, mimicking liver cell injury. This elevation is usually transient and harmless, but it can confuse the diagnosis.
- Stress: While severe psychological or physiological stress (like acute illness or major trauma) can affect the liver, ordinary daily stress is generally not considered a direct cause of elevated liver enzymes.
Q5: What does a high GGT level specifically indicate?
A high GGT (Gamma-Glutamyl Transferase) level is an important, sensitive marker used to confirm the source of liver stress.
GGT is concentrated in the liver cells and bile ducts. It is most often measured in conjunction with ALP (Alkaline Phosphatase):
- High GGT + High ALP: This pattern strongly indicates a cholestatic problem—meaning there is an issue with the flow of bile. This could be due to a blockage (like a gallstone or tumor) or damage to the bile ducts themselves (e.g., Primary Biliary Cholangitis).
- High GGT Alone: GGT is also extremely sensitive to alcohol consumption and certain medications. A high GGT level in isolation can be a specific indicator of recent or heavy alcohol use, or it can be elevated in conditions like non-alcoholic fatty liver disease, even when ALP is normal.
In summary, GGT acts as a critical confirmation test: it helps a doctor determine whether an abnormal ALP is coming from the liver/bile ducts (high GGT) or from other sources like bone disease (normal GGT).
Ready to gain clarity on your health? Click here to your essential health screening today! Book Now